The dental industry is investing heavily in the use of additive manufacturing, or 3D printing, as a more cost effective and sustainable method of producing dentures from medical-grade restorative materials. Most of the most well-known dental companies have a 3D printing research programme, with a view to limiting and ultimately terminating their traditional denture-based R&D offering in favour of a 3D printed solution. This, however, depends on advances in technologies and compliance with the latest industry regulations.
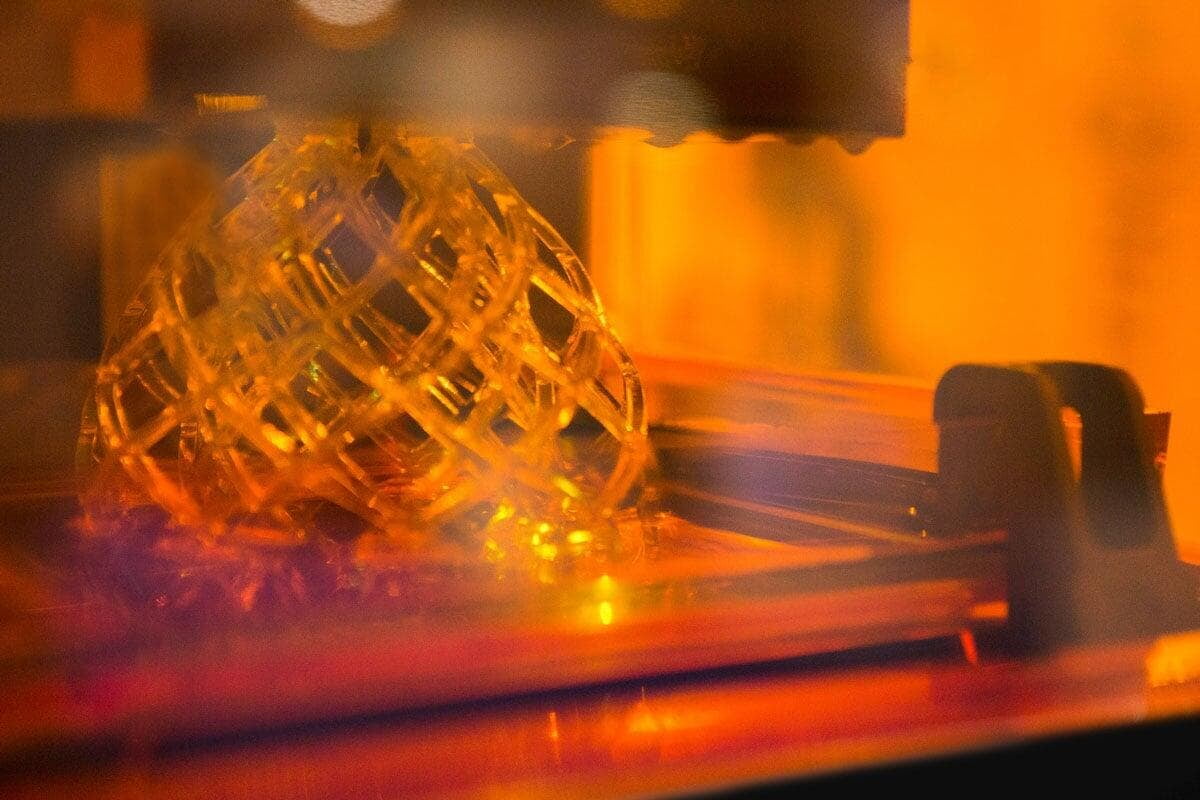
Stereolithographic printing in particular has been identified as the most promising form of 3D printing for the dental industry, because it offers the greatest accuracy and resolution, fine building details and a smooth surface finish. The technique involves a liquid thermo-set resin, which, using an ultraviolet laser curing device, cures the resin on the surface, layer by layer.
There has been a considerable amount of research into the specific use of stereolithographic 3D printing for dental restorative materials conducted across the world. A review of the most significant studies, 3D printing restorative materials using a stereolithographic technique: a systematic review, written by a team of researchers from the Postgraduate Program in Dentistry from the University of Passo Fundo, with support from the Department of Craniofacial Biology, at the University of Colorado, evaluates common research themes and combines conclusions for a comprehensive status report on the readiness of this technology.
What are researchers focusing on when studying stereolithographic printing?
This paper provides a qualitative analysis of studies focused on suitability of stereolithographic printing for denture manufacturing. It examines the dental restorative materials used in a range of studies, their properties, applied methods and the 3D printers used in each study.
Of the 47 studies included in the review, 38 used polymer-based restorative materials and the other nine focused on ceramic-based restorative structures.
The final printed structures were evaluated for a range of properties, with the three most common properties being dimensional accuracy which featured in 14 of the studies, strength (in 11 studies) and surface morphology (9 studies). Less common properties included antibacterial response, cytotoxicity, internal and marginal fit, fracture, wear resistance, density, viscosity, hardness, structural shrinkage and reliability.
The paper also describes how the printing conditions and, in some cases, chemistry affects certain characteristics. It highlights the importance of printing orientation, print angle and position, along with some of the technological challenges such as printing accuracy and the aesthetic appearance of the final product. These will all need to be overcome before the technologies are ready for mass adoption by the industry.
Identifying the barriers to progress
The research in this systematic review indicates that whilst demand from the dental industry is driving research into stereolithographic 3D printing of restorative materials, much work remains to be done to prove the viability of the product in application with patients.
Aesthetic appearance, wear resistance, wet strength and dimensional accuracy are the main current clinical limitations restricting the progression to functional part production with 3D printing.
Of the 47 studies reviewed, only five applied the printed dentures in patients, with the remaining 42 concentrating on proof of concept. The fact that only three studies considered parameters such as cytotoxicity, which is crucial to the implementation of the printed product into the mouth, is further proof that additional research and clinical trials are now needed.
What does this mean for the dental industry?
This summary paper identifies that the fast expansion of stereolithographic-based 3D printing has been impressive and represents great technological progress with significant disruptive potential.
There is a clear demand from the dental industry, and it is willing to adapt materials and adopt new ways of working to accommodate this promising digital technology.
However, overcoming the current clinical limitations during the proof-of-concept phase is crucial so that R&D departments can begin clinical trials and report on permanent/definitive dental restorative materials and structures.
1. A.D. Bona, V. Cantelli, V.T. Britto, K. F.Collares, and J. W. Stansbury, Dental Materials, 37 (2), 336-350 (2021). [https://doi.org/10.1016/j.