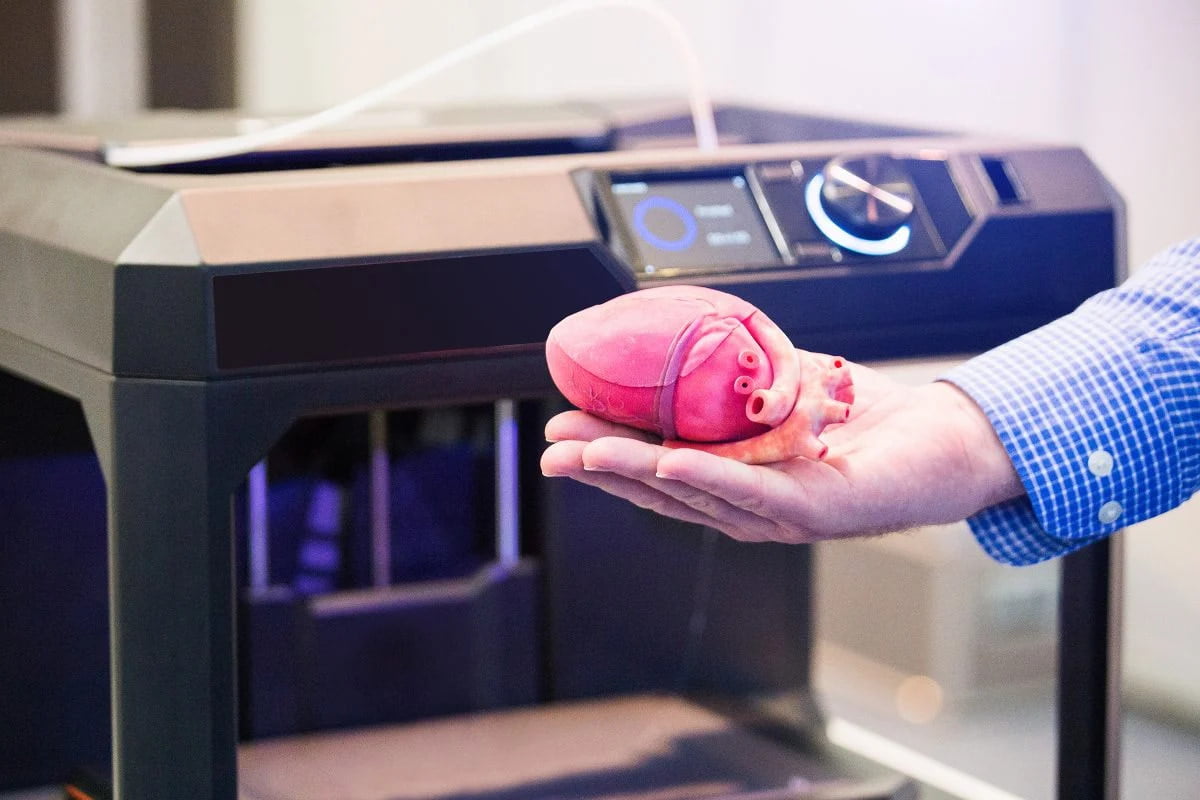
3D printing is a technology that can be used to quickly fabricate components of complex morphologies through the use of computational input. Accordingly, the use of computer-aided design (CAD) models of computed tomography (CT) scans can be employed as the basis for the 3D printing of medical equipment. The production of organ models, personalised tissue scaffolds and direct printing at a defect site can all be effected through the use of personal CT or magnetic resonance imaging data. In short, the development of this technique could furnish access to man-made tissues and organs, which would help to lessen the donor shortage problem.
Research for 3D printing applications in the medical sector falls into four classes:
- Production of pathological organ models to plan and aid surgery;
- Personalised manufacturing of permanent non-bioactive implants;
- The fabrication of local bioactive and biodegradable scaffolds; and
- Direct printing of tissues and organs with complete life functions.
Although these techniques are far from enjoying widespread medical use, some notable advances have been made, and are set out in brief below.
The reproduction of pathological organs for use by surgeons planning surgeries is a major area that plays to the advantages of 3D printing in terms of speed and cost, and the absence of tooling. Moreover, fabricated organs are not designed for implanting, so biocompatibility challenges vanish. Some researchers have developed a 3D-printed technique using cells and hydrogels that has furnished access to the interior structures of tumours for 3D imaging. Others have printed 3D anatomical models that contain high-resolution replicas of limbs, chest, abdomen, head, neck and other body parts that are ideally suited to medical training applications in hospitals. Further areas open to research in 3D-printed models extend to working with materials with different tactile elasticities, colours and compositions that approach more closely the appearances of human tissues and organs so that patients gain a better tactile experience from the models.
Dental and orthopaedic implants are the main areas of non-bioactive implants and 3D printing is optimal in these areas for customisation, speed, complexity and dimensional accuracy. This technique is now considered mature and is moving into the area of topological optimisation which allows the production of lightweight custom implants with adjusted stiffness. Recent developments have included the fabrication of custom joint and bone prostheses for osteosarcoma patients.
Biodegradable scaffolds form the structural bases of tissue-like architectures and are conventionally accessed through indirect and direct methods. Indirect cell assembly takes a pre-formed 3D scaffold which is then seeded with cells; in the direct cell process the cells and their structural repository are formulated together in a single go. The indirect cell assembly technique incorporates the cells into gel scaffolds. Gel scaffolds can be fabricated using several rapid manufacturing techniques, especially ink-jet based printing and offer the advantages of high water content, outstanding biocompatibility and controlled biodegradability, rendering them ideal for non-permanent applications. As such, inkjet-based bioprinting allows for very precise positioning of the biomaterials and cells. Direct cell assembly, on the other hand, requires careful control of cellular growth which is achieved by employing cellular dispersion in hydrogels; the scaffolds themselves which hold them are also gel-like in nature. Researchers working in 3D printed scaffold development have tailored many of the gel structures’ mechanical properties by using ionic, thermal and pH crosslinking. Typical outcomes have shown that ionic crosslinking removes excess mechanical energy, while covalent crosslinking provides routes to scaffolds with superior elasticity.
Finally, the direct printing of tissues and organs has already met with some success for the development of skin constructs, bionic ears and artificial tracheae. For other organs, the principal challenge lies in the incorporation of the vascular network necessary to create living structures. To this end, some research is now being directed towards the 3D printing of blood vessels.
Material selection and performance
3D-printable biomedical materials fall into three broad categories:
- Medical metals
- Medical polymer materials
- Medical ceramic materials
Medical metals, usually alloys such as cobalt-chromium, titanium or tantalum alloys are most often used for (dental and orthopaedic) implants. These compositions of materials offer good biocompatibility that satisfies medical standards. 3D-printed equivalents have the advantage of superior mechanical performance while allowing for customisation that can be tuned to match dental or orthopaedic properties. Some additional surface treatments, such as electrochemical or heat treatments, may enhance physicochemical properties still further.
Medical polymer materials are made from naturally-occurring polymers such as chitosan, collagen and fibrin. Such materials are ideally attuned to cellular proliferation and cell adhesion, but they deform easily and are of low mechanical strength. Synthetic polymers, such polylactic acid and polycaprolactone, offer the advantages of being precisely controlled during manufacturing but offer low compatibility for cell adhesion and proliferation. Hence, this is an area open to many enhancements. One area that has been examined has been antimicrobial composite resins that kill bacteria on contact without damaging human cells. This could be used for dental fillings.
Medical ceramic materials are mainly limited to hydroxyapatite (HA) and tricalcium phosphate (TCP). HA is a mineral component of bones and teeth and is ideally suited to 3D-printing techniques aimed at clinical applications. For dental applications, the control over shape, size and colour of implants that is afforded by the technique is ideal. Much work remains to be done in advancing the 3D printing of medical ceramic materials.
Considering the materials available for the 3D printing for medical applications, there remain many limitations. Many materials used for permanent implants have high elastic modulus which leads to an elastic mismatch between bone and implant. Printed biodegradable scaffolds fabricated with natural polymers have good biocompatibility but lack mechanical strength.